Pregnancy, Parenthood, and CPR Classes
Our mission is to educate, support and empower. Work with our team of licensed experts to gain confidence, master new skills, and connect with others.

Classes for Pregnancy
Prepare for the birth of your baby with our expert instructors.

Classes for Parenthood
Enhance your parenthood journey with classes around caring for newborns and young children.
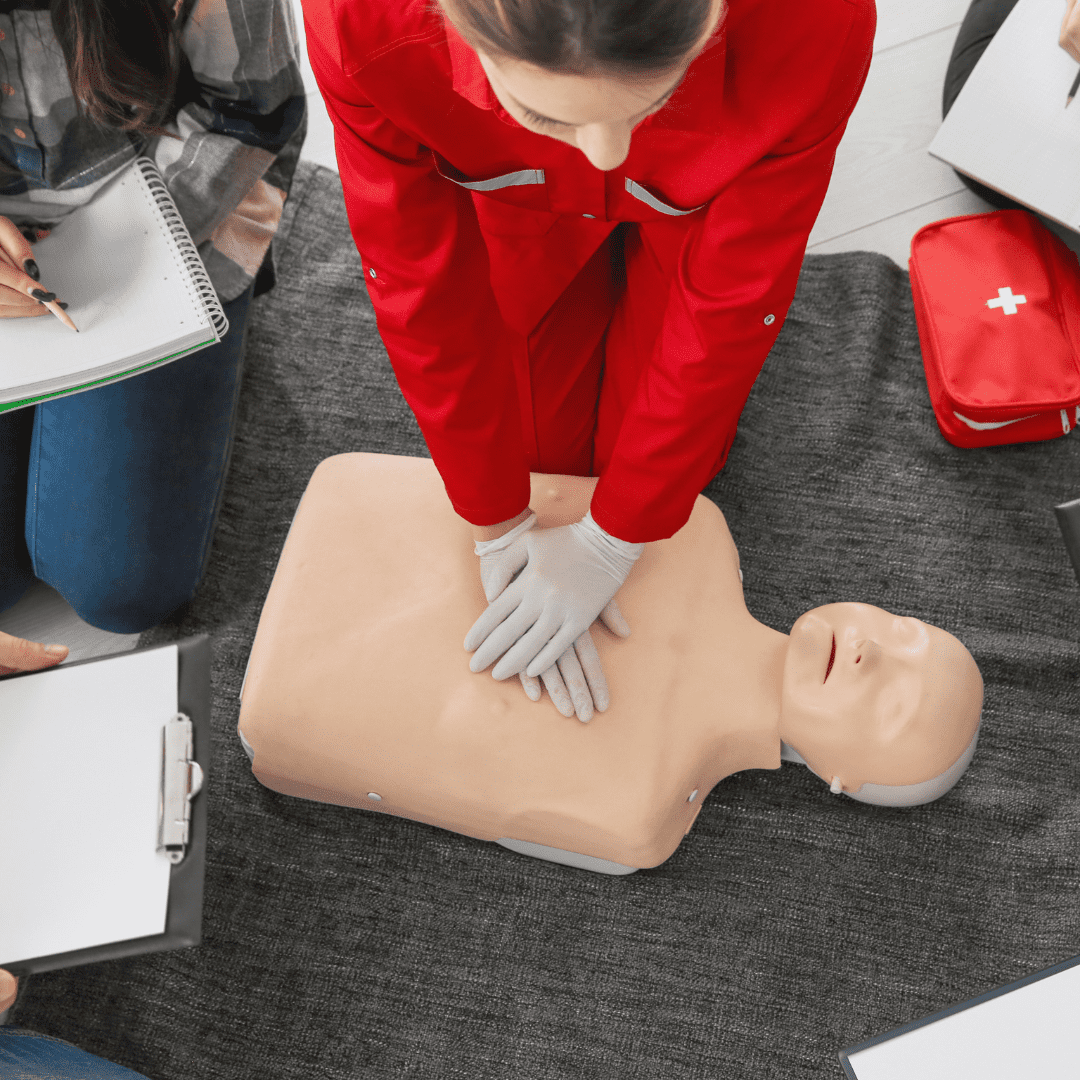
CPR Training and Certification
Learn these life-saving skills in CPR, AED use, and choking relief with Main Line Family Education.

Parent Connections and Support
Join us before or after baby to meet and connect with other new parents.

New Parent Support Package
Our New Parent Support Package provides families with private, virtual support during the first months of baby’s life.
What’s Happening at MLFEd





About Us
Main Line Family Education provides evidence-based education, support, and community for parents-to-be, young families, and anyone interested in learning life-saving CPR skills.
We are based 15 miles outside Philadelphia, in Devon, Pennsylvania. Classes are offered in-person in our Devon studio, virtually via Zoom, or on-demand via our website at a time that’s convenient for you. Our team of experts are specialized in the various class topics that they teach, and each live class is kept small to provide a more personalized educational experience.
At MLFEd we recognize that every pregnancy, birth, and family is unique. We offer small group classes, private classes at your location or ours, one-on-one new parent support and the opportunity to connect with other families. It truly does “take a village” and we’d love to be a part of yours!
What Our Parents Are Saying
“Main Line Family Education is a treasure! Nicole and her team give great advice and are always available for personal recommendations and tips. The courses that my wife and I have taken have been so insightful, helpful and reassuring and the team takes the time to make sure that it was easy to follow and understand all of the information. Don’t go through pregnancy and delivery without making use of this amazing resource.”
“My wife and I learned so much valuable information in classes with MLFEd. Our instructors, Nicole and Liz, were very enthusiastic when going over everything and super helpful answering questions. We took Breastfeeding 101 and Childbirth Preparation classes, and we are so grateful that we did. Seeing so much conflicting information online can be overwhelming. We enjoyed these classes and getting trusted information about what to do and expect. 10/10!!”
“We cannot thank Nicole and Main Line Family Education enough for all of the classes we have taken so far. We have done the Newborn Basics, Breastfeeding 101 and Childbirth Preparation classes and loved each and every one of them! They were all so informative and have both of us feeling much, much more prepared before our baby arrives! Nicole really does make Main Line Family Education feel like family and we are so happy to have found them and have them for any help in the future!”
“I’ve taken 4 classes with you now (time flies!), and I can honestly say you’ve helped make my transition as a new mom so much easier. I felt equipped to face many of the unknowns around childbirth, felt confident to know how to manage our breastfeeding relationship, learned about how to care for my body post-birth, and now helping my baby understand sleep and how to help him develop good sleep habits (gently!). I know not everyone’s experiences or babies are the same, and (mine) happens to be a very chill baby, but your classes let me be proactive in preparing all of us for the changes before we were desperate for help saving us from a lot of anxiety and stress.”
“My parents, husband and I all signed up to attend the Infant & Child CPR class through Main Line Family Education, and once again, we were so happy we chose to come here! Our instructor, Madison, was informative, outgoing and did a great job breaking down the information to us. The mixture of video, discussion, and hands-on practice was perfect to reiterate the information and make sure it stuck! It had been several years since I had learned CPR, so it was a great refresher while also learning new information with recent changes. We all left the class having peace of mind knowing our baby will be well taken care should an emergency arise!”
“I truly appreciate the expertise Erica brought to the class. It is so much less anxiety provoking to learn from someone who can tell you what the AAP recommends, but can also speak from experience and recognize that sometimes you have to do what is best for baby in the safest way possible….We have taken a few classes (CPR, Partners to Parents, Infant Sleep 101) and have found all to be helpful and worth the investment!”
“Liz did an absolutely fantastic job! I was engaged the whole time and never felt pressured to answer a question if I didn’t want to. She made me feel more confident and comfortable with the birth process. All of my questions were answered! I’m so thankful!”
“We took several classes with Main Line Family Education, both before and after our daughter was born. We took: Newborn Basics, Breastfeeding 101, Why Won’t My Child Sleep?! and Infant & Child CPR. Each class offered a unique expert with a wealth of knowledge. The classes are really small and individualized and we learned so much in each one! Nicole and her team are fantastic and we can’t say enough good things about them!”
“Nicole gave my husband and I such valuable information and allowed us to leave her Childbirth class with so much more confidence than when we came in. Her warmth and vast knowledge/resources made us feel at home and that we were in good hands. We are both so happy to have met her and to have had this experience be included in our journey.”
“Nicole is a great educator — she has mastery of the subject matter and breaks down information in an accessible way. I appreciate her combination of being positive and encouraging us to believe we can do it, while at the same time being realistic about the parts of childbirth and caring for newborns that are challenging and messy. Not everyone seems to get the “tone” right in a way that feels both empowering and realistic.”
This year, my husband and I were expecting our first child. I have always looked forward to taking birthing and parenting classes, etc. – just something weird I have always thought would be a fun experience. We took a couple Paoli hospital classes and another organization’s class (which were fine) but lackluster. Let’s just say they did not satisfy my craving.
Then we took a class with Nicole! Immediately the void was satiated; the interactive, educated, and overall positive and upbeat vibe that Nicole brought to the class, virtually, was fabulous. Both my husband and I feel that Nicole and guests provide the most well rounded, engaging, approachable parenting classes. I have continued on to attend many more MLFED classes since.
In a time when the world is having to keep distant, I have found friendship and a sense of community. I can’t say enough about how much Nicole has done for me and my family this year as an educator and a person. We are grateful for MLFED!
“I can’t recommend Nicole’s classes enough – we were looking for something different than the traditional hospital experience, but that would leave us ready to deliver at our Main Line Health hospital. Nicole offered just that. With her years of experience and vast knowledge of what it’s really like…we felt cared for and informed. If you’re looking for a smaller feel in a beautiful location, Main Line Family Education is absolutely the way to go!”
“Tremendous experience. My wife and I attended a five-hour session on Sunday (Childbirth Preparation) and cannot rave enough about the program. We learned so much, but more importantly feel so much more comfortable and prepared to start this new journey. The instructor’s expertise was paramount in the session, and I can honestly say she put many fears at ease.”
“I was so impressed with the instructor and the way she taught the class. My experience was awesome . I was so glad to have the models to practice on and see the immediate feedback from the blinking lights. The instructor was excellent and everyone seemed comfortable and actively engaged. I was able to practice as much as I wanted and I am now confident that I can use these skills in an emergency. Thank you!”
My wife and I recently attended a Childbirthing Prep class taught by Nicole here. The space was very upscale and comfortable, and Nicole was both engaging and knowledgeable. As first time parents, this was a must-take class for us. I’m sure we will be back soon for more. Thank you Main Line Family Education!
“We cannot thank Nicole and Main Line Family Education enough for all of the classes we have taken so far. We have done the Newborn Basics, Breastfeeding and Childbirth Prep classes and loved each and every one of them! They were all so informative and have both of us feeling much much more prepared before our baby arrives! Nicole really does make Main Line Family Education feel like family and we are so happy to have found them and have them for any help in the future!”
“It is clearly evident which parents have truly prepared for the birth of their child. I took care of a super cute couple that delivered at Lankenau and took classes with you. I remember that they were first-time parents, but confident. They had their act together! That’s why I asked them if they had prepared — and they mentioned your program at Main Line Family Education.”
“This was the third class I’ve taken with MLFEd and it was just as good as the others. It’s great to be able to learn from people with real life, hands-on experience. Everyone is so friendly and helpful.”
“I have been looking forward to this class [Nutrition for Pregnancy] and was very happy to hear Jacqueline was coming back from maternity leave. As the class wasn’t available until the end of my second trimester, I bought a nutrition book early on in pregnancy and while it covered macro and micro-nutrients, Jacqueline’s personal knowledge highlighted so much more of what I wanted and needed to hear. I am thrilled with the wealth of information I walked away with.”
“The [Pelvic Floor, Core & More] instructor was fantastic. Essential information that everyone should know when becoming a mom. Thank you so much for offering this!!!”
Main Line Family Education, LLC
34 Berkley Road
Suite 200
Devon, PA 19333
info@mlfed.com
484.254.6581
More Information
Location
Serving clients in Devon, PA and surrounding areas, including Malvern, Paoli, Berwyn, Wayne, Radnor, Villanova, Bryn Mawr, Havertown, King of Prussia, West Chester, Downingtown, Exton, and Center City Philadelphia.
Virtually serving clients throughout the United States, including Delaware, New Jersey, New York, Ohio, Maryland, Virginia, Illinois, Washington, Texas and California.
Virtually serving clients internationally in Canada, Europe and Asia.